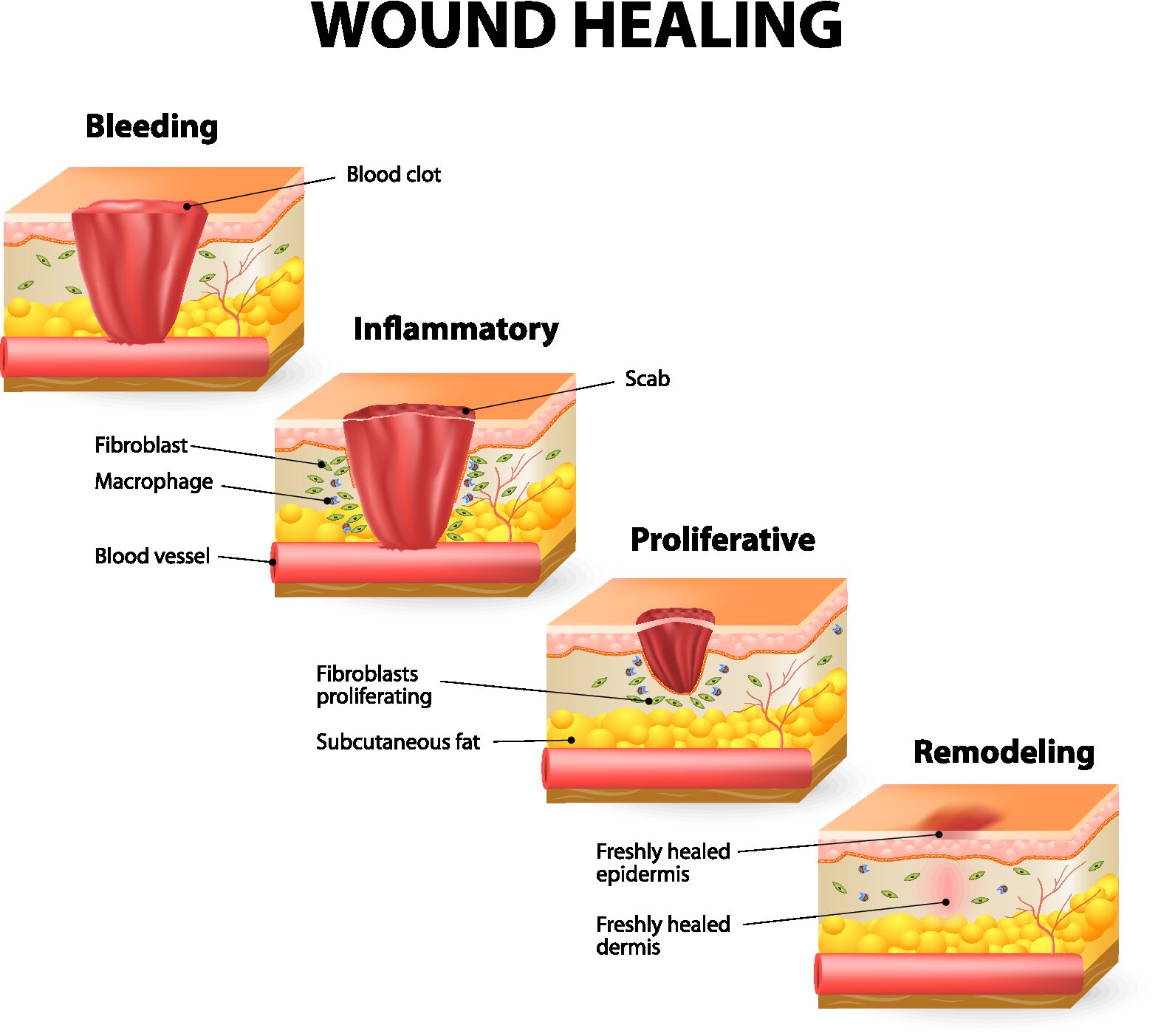
The process of wound healing can be divided into four main phases:
Hemostasis: The first phase of wound healing is hemostasis, which begins immediately after the injury occurs. During this phase, the body tries to stop bleeding and form a blood clot to seal the wound. Platelets and clotting factors in the blood are activated, which helps to form a clot and prevent further blood loss.
Inflammatory phase: The second phase of wound healing is the inflammatory phase, which typically lasts 2-5 days. During this phase, the body sends specialized cells to the wound site to remove debris and fight off infection. The wound becomes red, swollen, and painful due to increased blood flow and the presence of inflammatory cells.
Proliferative phase: The third phase of wound healing is the proliferative phase, which usually begins on day 3 or 4 and can last up to 3 weeks. During this phase, new tissue is formed to replace the damaged tissue. Blood vessels grow into the wound, and fibroblasts produce collagen, a protein that gives strength and flexibility to the new tissue.
Remodeling phase: The final phase of wound healing is the remodeling phase, which can last for several months to a year or more. During this phase, the new tissue is remodeled and strengthened. Collagen fibers are realigned, and the wound gradually becomes stronger and more like the surrounding tissue.
During the inflammatory phase of wound healing, which typically lasts 2-5 days and up to 2 weeks, the body sends specialized cells to the wound site to remove debris and fight off infection. This phase is characterized by a series of events that occur as part of the body’s immune response to injury:
Vasoconstriction: Immediately after injury, blood vessels in the area constrict to reduce bleeding and prevent further damage. Vasodilation: After the initial vasoconstriction, blood vessels in the area of the wound dilate, allowing more blood and nutrients to reach the site of injury. Increased permeability: The blood vessels become more permeable, allowing white blood cells and other immune cells to migrate from the bloodstream into the surrounding tissues. Migration of immune cells: Neutrophils, macrophages, and other immune cells migrate to the wound site to phagocytose (ingest and destroy) bacteria and debris. Release of cytokines: The immune cells release cytokines, which are signaling molecules that help to regulate the inflammatory response and stimulate the proliferation of new cells. Swelling and pain: The release of cytokines and other inflammatory mediators causes swelling, redness, and pain at the site of the wound.
Overall, the inflammatory phase of wound healing plays a critical role in removing damaged tissue and preventing infection, laying the foundation for the subsequent phases of wound healing.
During the proliferative phase of wound healing, new tissue is generated to fill the wound space. This phase usually begins around 3 to 5 days after the injury and can last up to 2-6 weeks. The main events that occur during this phase include:
Angiogenesis: The formation of new blood vessels in the wound area, which provides oxygen and nutrients to the healing tissue. Granulation tissue formation: The proliferation of fibroblasts, which are cells that produce collagen and other extracellular matrix components. The fibroblasts migrate to the wound area and produce a granulation tissue that fills the wound space. Contraction: The wound edges begin to pull together as myofibroblasts (specialized fibroblasts) contract the wound. Epithelialization: The migration and proliferation of epithelial cells from the wound edges, which form a new layer of skin over the wound. Maturation: The newly formed tissue gradually gains strength and flexibility as the collagen fibers reorganize and cross-link.
All these processes in the proliferative phase are necessary for the wound to close and for normal skin function to be restored.
The remodeling phase of wound healing is the final stage in which the newly formed tissue undergoes maturation and reorganization to achieve maximum strength and function. This phase begins after the wound has been closed and can continue for several months or even years. During the remodeling phase, the following events occur:
Collagen remodeling: The collagen fibers that were laid down during the proliferative phase are reorganized and cross-linked to increase the strength and flexibility of the tissue. Scar formation: The granulation tissue gradually transforms into scar tissue, which is composed of a dense network of collagen fibers. Vascular maturation: The newly formed blood vessels undergo maturation and remodeling to become more organized and functional. Tissue contraction: The wound continues to contract, which may result in further changes to the appearance of the scar.
Overall, the remodeling phase is crucial for achieving the final appearance and function of the healed tissue. The strength and flexibility of the new tissue continue to improve over time, and the scar may become less noticeable as the collagen fibers mature and reorganize.
Manual lymphatic drainage (MLD) is a therapeutic skin-stretch technique that can help to reduce swelling and inflammation, increase lymphatic flow, and promote healing. Here’s how MLD may help during the different phases of wound healing:
Hemostasis phase: During this phase, MLD may help to reduce swelling and edema around the wound site, which can help to minimize further damage and improve circulation to the area.
Inflammatory phase: MLD may help to reduce swelling and inflammation at the wound site, which can help to speed up the healing process and reduce pain and discomfort. By promoting lymphatic flow, MLD can also help to remove waste products and cellular debris from the wound site, which can help to prevent infection.
Proliferative phase: MLD may help to promote the growth of new tissue and improve circulation to the wound site, which can help to increase oxygen and nutrient supply to the area. By stimulating lymphatic flow, MLD can also help to remove excess fluid and reduce scarring.
Remodeling phase: During this phase, MLD can help to reduce scar tissue formation and promote healing of any residual inflammation. By promoting lymphatic flow, MLD can also help to reduce the risk of lymphedema, a condition that can occur when there is impaired lymphatic drainage.
Overall, MLD can be a useful adjunct therapy during wound healing, particularly for individuals who are at increased risk of lymphedema or have impaired lymphatic flow.
The timing of starting manual lymphatic drainage (MLD) after plastic surgery can vary depending on the specific surgery, the extent of the procedure, and the surgeon’s preference. In general, MLD can be started as early as 24 to 48 hours after surgery.
However, it is important to consult with your surgeon before starting MLD to ensure that it is safe and appropriate for your specific situation. Your surgeon may recommend waiting for a certain amount of time before starting MLD or may suggest a different type of postoperative care.
Additionally, it is important to seek out a qualified and experienced therapist who is trained in postoperative MLD techniques. The therapist can work with your surgeon to develop a customized treatment plan to address your specific needs and ensure a safe and effective recovery.